Welcome to the new Big Data for Better Care Homes blog. My name is Dr. Fiona Headley and I am a Knowledge Transfer Partnership (KTP) Associate in Medicines Data Analytics with Cardiff University and Invatech Health Ltd, a healthcare technology company headed by pharmacist Tariq Muhammad. The aim of this project is to build a product using big data analytics to support medicines optimisation in care and nursing homes. In this introductory article, I will explain more about the KTP project and why I am passionate about this.
About Me
I began my career working as a care assistant in a residential home in Somerset. I then completed both a BSc in Global Public Health and my MBBS degree at Barts and the London School of Medicine and Dentistry. Following this, I worked in the NHS as a junior doctor. It was during this time that I developed an increasing interest in healthcare technology and how this can be used to improve care, clinical outcomes and efficiency. I also feel that, despite being a key contributor to the wellbeing of particularly vulnerable groups, the social care sector is often overlooked. Therefore, I am very excited to be a part of this project to integrate clinical care, social care and technology.
What is the problem?
Polypharmacy is common in care homes. The Department of Health Care Home Use of Medicines Study (CHUMS) 2009 found an average of 8 items prescribed per resident. Greater numbers of medicines increase the risk of errors. In the same study, approximately 70% of all residents were found to have a medication error, almost 40% experienced a prescribing error and almost 20% of patients on at least one drug needing monitoring were not being monitored properly. These are commonly a result of human error and can have devastating outcomes. The risk and potential consequences of human error is highlighted by Dr Prabhu in the Topol review, who advocates for the use of technology to reduce the chance of this occurring.
Care home residents have also been shown to be more likely to receive high-risk medicines. For example, the Quality of Prescribing in Care Homes and Community in England and Wales study, 2012 found care home residents were more likely to receive anticholinergics and antipsychotics compared to community dwelling elderly.
Medicines management in care homes is complicated by complex needs, multidisciplinary teams and often an inability of the resident to attend a GP surgery. In recognition of this, recently Enhanced Care for Care Homes vanguards have been established, with the aim of improving integration between health and care services to improve outcomes. The NHS England framework on this recommends medicines review at least yearly, focusing on safety, and a proactive approach to care using business intelligence and health analytics to identify care home residents at high risk unplanned hospital admission.
What is the idea?
Invatech Health Ltd produce an eMAR system called Atlas, which uses barcode technology and handheld devices to dispense and administer medicines; and monitor stock control. This is linked to the pharmacy, so that the care home and the pharmacy have up-to-date, synchronised information. Find out more here.
The Knowledge Transfer Partnership project has developed following research conducted by Cardiff University on the safety and efficiency of Invatech Health’s Atlas eMAR system, which found the Atlas system to eliminate 21/23 administration errors. It is a 3-year government initiative, running until 2022, which aims to use the big data collected by Invatech Health’s system to improve clinical outcomes, prescribing safety and quality of care.
An idea for an initial starting point with this is to develop a business intelligence dashboard for clinical medicines management in care homes, similar to the type that is used for monitoring medicines management at CCG level. However, the aim by the end of the 3 years is to go further than this and use machine learning methods to predict the risk of outcomes related to medicines use, for example falls.
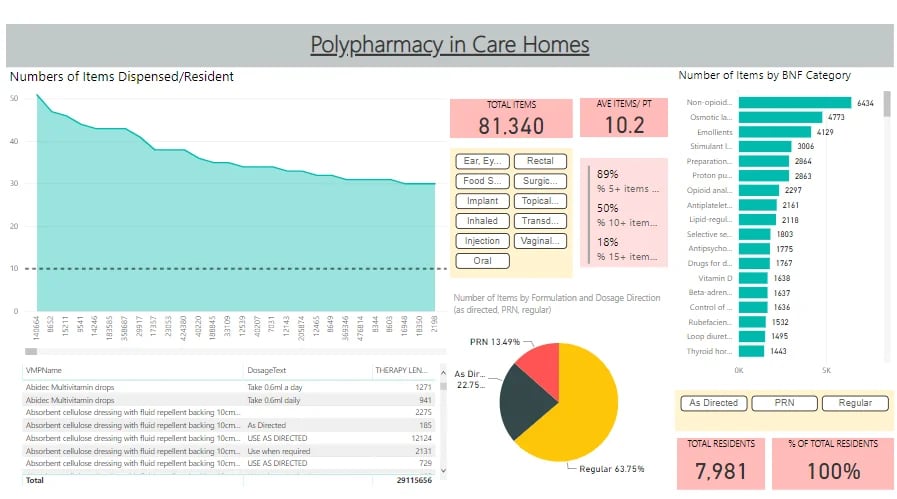
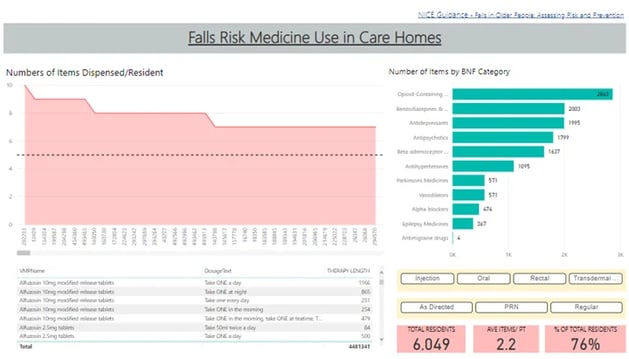
The images show some screenshots of initial work on how business intelligence dashboards for polypharmacy and falls could look. They are dynamic – for example in the polypharmacy dashboard, if you click on the oral button then only oral medicines will be shown. This could be used in GP practices or by pharmacists, filtered to only the individuals they care for, to highlight those at greatest risk from polypharmacy and falls risk medicines.

Why is it important?
As previously mentioned, errors are common and so safety is a primary concern.
It is also important to recognise the current climate in health and social care. Funding in adult social care has fallen 1.5% per year since 2009/10, while the age-adjusted per-person spend on health has risen only 0.1% per year. Coupled with an ageing population with increasing multimorbidity and polypharmacy, this is leading to an increasing spending-funding gap, which is estimated to be £34bn in the NHS and £8bn in social care by 2033/34.
Meanwhile, there is an ongoing staffing crisis. For example, approximately 10% of registered nurse and care worker roles in adult social care are unfilled, and there are similar shortages of staff in the NHS. The number of unfilled vacancies is compounded by individuals leaving the profession. For example, a 2018 GMC commissioned independent survey of its members found over 1/3 of GPs were planning to leave and over ¼ planning to reduce hours in the near future. The potential to use technology to improve efficiency is recognized by GPs, with over ¾ surveyed having considered smarter working practices using technology to gain efficiencies.
Technology has the potential to not only improve efficiency, but also improve quality of services. For example, a shared platform for medicines management would strengthen the partnership between care homes and clinical staff, allowing for better integration and collaboration. Such an approach of a GP-led MDT supported by technology has been recommended by the Primary Care Workforce Commission, 2015 as delivering best primary care. Advanced data analytics could provide risk stratification to allow care to be proactive as well as reactive. Furthermore, the use of technology to improve efficiencies frees up healthcare professionals to focus on the person.
Conclusion
This blog will follow the journey of the KTP project to use big data analytics to provide clinical insights. As part of this, I will be taking a variety of clinical areas, researching and summarizing current guidance for best practice and exploring the data in relation to this. There is also opportunity to get involved. There will be more details about this in an upcoming blog.