There has been a recent surge in the recognition of the pivotal role that innovation, digital healthcare and technology will play in the quality and sustainability of health and social care in the UK. This has been highlighted in the NHS long-term plan, the discussions surrounding the social care Green Paper, and frequently by Matt Hancock since his appointment as Secretary of State for Health and Social Care. It is then detailed further in the Topol review; in the government policy paper, The future of healthcare: our vision for digital, data and technology in health and care; and in the work of NHS digital. This article will take a look at the governments’ future vision for health and social care, with a focus on the role that technology will play in achieving this.
What is the governments future vision for the NHS and social care?
The NHS Long Term Plan
Marking the NHS’ 70th anniversary, the NHS Long Term Plan outlined “three big truths”:
- Pride in the enduring success of the NHS
- Concern about funding, staffing, increasing inequalities and the pressures of a growing and ageing population
- Optimism for continuing advancement and improving outcomes
The NHS Long Term Plan coincides with the promise of a greater yearly increase in funding, from 2.2% to 3.4%. It emphasizes the need to optimize the use of this funding. It also highlights the disparity between workforce growth and increasing demands, and the need to support and expand the workforce. It describes how these will be tackled be redesigning patient care. This includes a focus on out-of-hospital care, reducing pressure on emergency hospital services; enhanced integration between health and social care; improved personalization of care; and digitally-enabled services. There is also a focus on population health and disease prevention, for example smoking cessation, obesity and alcohol excess, alongside major health conditions such as diabetes, stroke care and adult mental health.
The Social Care Green Paper
Initially announced in March 2017, the publication of the social care Green Paper has been long awaited. Since the original plan to publish this in the Summer of 2017, the publication date has been delayed five times. In a speech just two weeks after his appointment as Secretary of State for Health and Social Care, Matt Hancock said “we’re committed to a comprehensive green paper on social care in the autumn”, and later in January this year said this would be before April. Sadly, this has still yet to come to fruition.
A hint of what it is likely to contain was given by Jeremy Hunt in March 2018 and again in the Social care: forthcoming Green Paper (England) House of Commons Briefing Paper. The Government have stated this will cover all ages of adults, both working age and over retirement age, covered in two separate streams. In his speech in March 2018, Jeremy Hunt outlined “the seven key principles that will guide our thinking ahead of the Green Paper”, namely:
- Quality – putting care to the “good enough for my mum” test.
- Whole-person integrated care – health and social care working together to provide integrated care, centered around the individual.
- Control – giving the individual and families the funding and transparent, reliable information to make informed choices.
- Workforce – increase in the National Living Wage, promoting career building and recognition of social care workers as “our society’s modern-day heroes”.
- Supporting families and carers – to recognize the contribution of carers, improve support and “make the needs of carers central”.
- A sustainable funding model supported by a diverse, vibrant and stable market – sourcing additional funding; investment in and system wide dispersal of technologies and innovation; and allowing choice of quality, cost-effective services.
- Security for all – celebration of social care’s 70th birthday and continued commitment for the National Assistance Act’s principle of a “shared responsibility for care”, while addressing inequities in the state support provided to individuals.
How will technology be used to help achieve this?
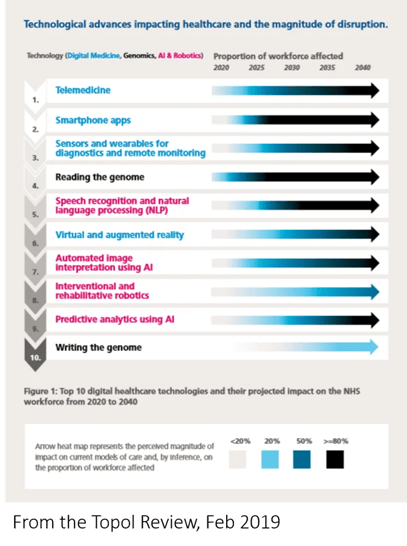
Technology has been recognized as central to achieving the governments’ future vision for health and social care. In fact, this is one of Matt Hancock’s three priorities for the health and social care, alongside the workforce and prevention. The Topol review gives detail about the top health and care technologies and the potential benefits of adaptation of these digital healthcare and technologies. It also gives guidance on progressing these and disseminating evaluated, evidenced technologies throughout the health and care systems.
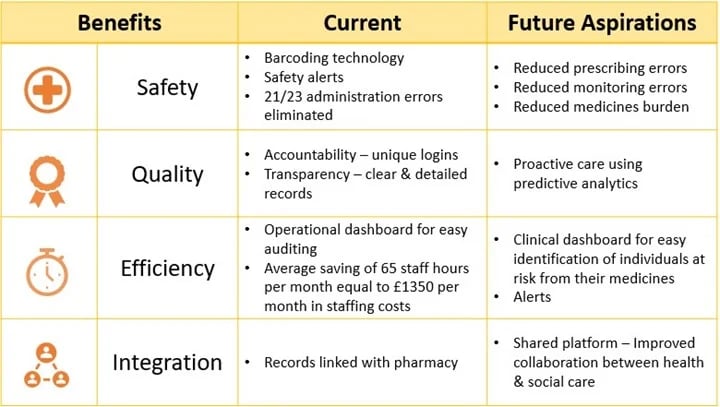
The main ways in which technology has been highlighted to support the future vision of health and social care are integration, efficiency, safety and quality.
Integration
Integrated care is recognized as vital for improvement of illness prevention and thus reducing burden on NHS services. The NHS Long Term Plan aims for Integrated Care Systems to be widespread by April 2021. It envisages a future where clinicians can easily access patient records and care plans wherever they are. Where predictive techniques are used to support decision and the work of Integrated Care Systems. As part of this, Primary Care Networks are being established. These will be multi-disciplinary teams aimed at offering targeted support to those with specific conditions at greatest risk such as dementia and to improve prevention of adverse outcomes, for example from falls. For effective integration of services digital maturity needs to be widespread and systems interoperable. Therefore, these are mentioned as key areas of focus.
Efficiency
Another key area where there is an emphasis on the use of technology is in improving efficiency and therefore making the most out of limited resources. One suggestion for this in the NHS Long Term plan is to utilize the digital data captured to reduce the administrative burden of staff. The NHS Long Term Plan also describes how technology can save time for patient through the digital-first primary care, which will give every patient the right to choose remote care online or by telephone; and through a streamlined service for specialist advice supported by technology. Meanwhile, the Local Government Associations describes how improved use of data analytics can improve spending by predicting outcomes and taking early interventions.
Safety
There has also been a focus on safety. In his speech following the publication of the Topol review, Matt Hancock stated “I care about tech because I care about people”. He emotively describes Dr Prabhu’s experience with the devastating effects human error can have when this occurs in health and social care. The NHS Long Term Plan highlights the ability of technology to provide safety prompts. There also needs to be safety and security of patient data, as highlighted in the government policy paper, The future of healthcare: out vision for digital, data and technology in health and care.
Quality
Finally, technology and innovation has been recognized to be a key contributor to future improvements in the quality of health and care services. For example, the use of decision support and artificial intelligence can not only improve efficiency, but also support best practice, reducing inequities in quality of services. Data can also be used to more easily and efficiently assess effectiveness of interventions. Meanwhile, a focus of prevention supported by data science techniques has the potential to advance health and care outcomes. For example, the Topol review describes how predictive analytics based on machine learning techniques have been shown to provide more accurate predictions than traditional clinical risk scores. Finally, the Topol review emphasizes how improvements in efficiency will free up staff to focus on the ‘uniquely human’ aspects of health and care.
How does this fit with ATLAS eMAR and the Big Data for Better Care Homes project?
The benefits described in these government papers fits with those that have been experienced when digitizing medicines management. The table included details the current evidence for these benefits through using ATLAS technology for medicines management, and the aspirations for future further improvements in these through the Big Data for Better Care Homes project. This includes previous studies by Cardiff University examining the safety and efficiency of ATLAS have shown this system to eliminate 21/23 medication errors and improve efficiencies, resulting in average time savings of 65 hours per month.
Conclusion
Digital healthcare and technology are likely to play an increasingly significant role within health and social care. This has the potential to support health and social care sustainability and improve quality, safety and efficiency of services. To reach its full potential, the use of these technologies needs to be embraced by a digitally trained workforce throughout health and social care. Sadly, although the importance of technological advancement has been highlighted for both health and social care, most of the documentation probing further into the specifics of this relates to health and the NHS. Hopefully this detail will be provided in the long anticipated social care Green Paper.
Want to find out more?
Get in touch if you have any questions or would like to discuss ATLAS eMAR in more detail.